
Clinical aspects of pregnancy and parturition of the pregnant women with tuberculosis of respiratory organs: retrospective, case-control study
RESEARCH ARTICLE
Clinical aspects of pregnancy and parturition of the pregnant women with tuberculosis of respiratory organs: retrospective, case-control study
Zoreana Cazacu1†*, Olga Cernețchi1†
1Chair of obstetrics and gynecology no. 2, Nicolae Testemitanu State University of Medicine and Pharmacy, Chisinau, Republic of Moldova.
Corresponding author:
Zoreana Cazacu, PhD student
Chair of obstetrics and gynecology no. 2
Nicolae Testemitanu State University of Medicine and Pharmacy
165, Stefan cel Mare si Sfant ave., Chisinau, Republic of Moldova, MD-2004
e-mail zoreanacazacu@gmail.com
Short title: Tuberculosis and maternity
What is not known yet, about the topic
The particularities of evolution of pregnancy and parturition, incidence and structure of perinatal morbidity and mortality in women with tuberculosis of the respiratory organs, depending on the clinical form of the specific process.
Research hypothesis
Analysis of particularities of evolution and conduct features of pregnant women with tuberculosis of the respiratory organs in conditions of direct observed therapy monitoring.
Article’s added novelty on this scientific topic
The study allowed to clarify the peculiaritites of pregnancy, parturition and post-partum evolution; incidence and structure of perinatal morbidity and mortality in women with tuberculosis of respiratory organs according to the clinical form and gestation term at the time of specific process detection.
ABSTRACT
Introduction. The risk of maternal and perinatal pathology in pregnant women with active tuberculosis of respiratory organs significantly increases. The purpose of the research, was to make a comparative evaluation and analysis of the peculiaritites of pregnancy and parturition evolution, incidence and structure of perinatal morbidity and mortality in women with tuberculosis of respiratory organs, according to the clinical form of the specific process; optimization of pregnancy and parturition conduct in this contingent of patients.
Material and methods. The retrospective study was at the basis of this work, case-control type of 239 patients between the ages of 17-46 years, divided in 2 groups, according to the contraction of the tuberculous infection during pregnancy. The research was conducted by examining medical documentation (obstetrical observation card, new-born card). The data were numbered in Excel tables. Was applied the χ² test, for comparing the categorical variables, in groups. A p<0.05 was considered statistically significant.
Results. An increased incidence of pregnancy complications (feriprive anemia, imminence of spontaneous abortion, imminence of premature birth, pathology of the fetus-placental system) and parturition (prenatal rupture of the amniotic sac, rapid and fulminant birth, maternal obstetrical trauma, insufficient contraction forces) was ascertained in women with active tuberculosis of respiratory organs – up to 70% cases, in comparison to pregnant women without tuberculosis. The evaluation of the new-borns, has diagnosed neonatal pathologies such as intrauterine infection, aspiration syndrome, congenital developmental abnormalities, aspiration pneumonia, haemorrhage/peripheral ischaemia, ischaemic hypoxic encephalopathy and intrauterine growth retardation of the fetus significanty, more frequently in the group of pregnant women with active tuberculosis of the respiratory organs in comparison to pregnant women without tuberculosis.
Conclusions. In our research was demonstrated the unfavorable action of tuberculosis on the process of gestation, which is also reported in the specialty works, namely according to the form and phase of the specific process.
Key words: pregnancy, parturition, tuberculosis of respiratory organs, pregnant women, perinatal results.
INTRODUCTION
Even if the disease is treated earlier, TB causes morbidity and mortality. TB during pregnancy is not an exception. Despite the prompt treatment, TB negatively affects both maternal and perinatal results. However, the negative resuls of pregnancy are more pronounced in cases of late diagnosis, advanced disease, incomplete and / or irregular treatment [1]. The data on the effects of TB on the maternal and neonatal results are contradictory. Mnyani C. et al. (2011), suggested that the treatment of TB in a timely and appropriate manner dosen’t have a negative effect on the pregnancy results [2], while Lin H. et al. (2010), suppose that TB in pregnant women is associated with the negative results of pregnancy [3]. The gloomiest prognosis was recorded in women with advanced form of TB in the puerperal period, as well as in those with HIV co-infection. Reduced adherence to treatment also aggravates the prognosis [4, 5].
Most scientists believes, that in case of early diagnosis and appropriate treatment, the morbidity and mortality rates are significantly reduced and the evolution of pregnancy is not changed by TB [6, 7]. There is no statistically significant increase of congenital malformations in children born by mothers with TB, though the prematurity, intrauterine growth retard of the foetus, small weight at birth and perinatal mortality were frequently reported by Ali A. et al (2011) [8]. The risk of having small children at the gestational age was of 2.6 and it appears in about 20.2% of pulmonary TB cases and in approximately 33% of extrapulmonary TB cases [6].
Mayer K. et al. (2012), think that the most aggressive during pregnancy is TB [9]. For these reasons, the management of TB in pregnant women and breast-feeding mothers has a special importance. The early treatment of the pregnant woman with TB reverses the negative impact on the perinatal results [9, 10, 11]. The TB diagnosis in pregnant women is often overdue, because of the symptoms and signs similar to those of pregnancy, resistance of doctors and refuse of the patients to make X-ray investigation to pregnant women and relative difficulties of access for biopsy of affected organs, especially, in extrapulmonary injuries. A high suspicion and the early investigation for TB during pregnancy contributes to a better detection of TB.
The purpose of the research was the assessment and comparative analysis of evolution peculiarities of pregnancy and parturition, incidence and structure of perinatal morbidity and mortality in women with tuberculosis of respiratory organs according to the clinical form of the specific process.
MATERIAL AND METHODS
During the years 1999-2009, the research was conducted at the basis of the chair of obstetrics and gynecology no. 2, Nicolae Testemitanu State University of Medicine and Pharmacy, Municipal Clinical Hospital no. 1 and Institute of Mother and Child.
The protocol of the present study was approved by the Research Ethics Committee of the Nicolae Testemianu State University of Medicine and Pharmacy, at the meeting of September 17, 2012.
The investigation was conducted by examining the medical documentation (obstetrical observation card – form no. 96/e, new-born observation card – form no. 003/e).
The basis of the research was the study case-control of 239 patients, divided into 2 groups, according to the contraction of tuberculous infection during pregnancy:
- group with TB – 120 pregnant women, who contracted specific infection (LB);
- No TB group – 119 pregnant women, almost healthy, without tuberculous infection (LM).
The women from the group with TB were divided, accordging to the activity of the tuberculous process, in 2 subgroups (LBA – pregnant women with an active form of the tuberculous process and LBS – pregnant women with sequelae of the tuberculous process).
The sample size was determined according to the formula:
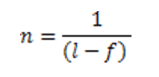
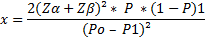
where:
n – sample size;
P0 – proportion of births in women with TB in general population, according to statistics 0.5 in 100 births;
P1 – proportion of births in women with TB in the study group, suppose will be three times more frequently than the general population (RP=3).
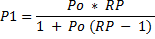
where:
RP – probability ratio.
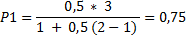
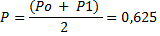
1-P=0,325
When the statistical power β equals to 5%, then the coefficient Zβ=1,65.
When significance threshold is equal to 0.05, then the coefficient Zα=1,65 (from that table).
f – number of persons who abandoned the study, supposed up to 10%.
Introducing these values in the formula we got:
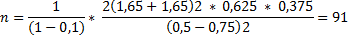
Thus, in the basic group there should be no less than 91 of pregnant women with TB of respiratory organs.
In the study, all the cases of deceased new-borns, in terminal phase and spontaneous abortions, were excluded. The women with insufficient information for establishing the date and way of pregnancy resolution were excluded from the study. The following pregnancy aspects in pregnant women with TB of respiratory organs were addressed: peculiarities of obstetrical, gynaecological and somatic anamnesis, social and demographic characteristics, clinical evolution of pregnancy and parturition, the nature of complications, data about the condition of the new-borns, ratio of breastfeeding and the ratio of vaccination with BCG.
The diagnosis of TB of the respiratory organs in pregnant women was established on the basis of clinical, epidemiological, biochemical, serologic and imaging data. The active TB is manifested with clinical signs and symptoms characteristic to TB, this includes the following main sindroms: general intoxication syndrome (nightsweats, subfertility or long standing fever, fatigue, general weakness, asthenia, decreased appetite, body weight loss) and bronchopulmonary syndrome (persistent cough 3 weeks with or without expectorations, haemoptysis, pain in the thoracic cage, dyspnoea). The patients with sequelae of the TB process show no signs and clinical symptoms characteristic for TB, above mentioned, the tuberculous infection being contracted and treated in anamnesis with at least one year until the moment of gestation.
The data were numbered in Excel tables. Was applied the test χ² for comparing the categorial variables, in groups. A p<0.05 was considered statisticaly significant.
RESULTS
The average age was 26.9±0.6 years in women from LBA, 27.3±0.7 years in women from LBS and 27.9±0.5 years in women from LM.
Most of pregnant women included in the study had optimal reproductive age for pregnancy and delivery – 17-39 years – 233 (97.5%) women.
Gestation analysis revealed that in all study groups prevailed the multigestation pregnant women (pregnant women with 3 and more pregnancies): 53 – 63.9% in LBA, 29 – 76.3% in LBS and 65 – 54.2% in LM.
In the group of pregnant women with active tuberculosis, primiparous were 36 (43.9%) persons, secundiparae – 29 (35.4%), and multiparae – 17 (20.7%). In the control group, there were 66 (55.5%) primiparous, secundiparae and multiparae had a ratio of 35.3% and 9.2% cases, respectively.
The pregnant women with active TB of respiratory organs were under supervision at the tuberculosis dispensary with the following clinical forms of TB: infiltrative pulmonary TB – in 52 (63,4%) cases, nodular pulmonary TB – in 4 (4,9%) cases, disseminated pulmonary TB (miliary) – in 6 (7,3%) cases, fiber-cavity pulmonary TB – in 5 (6,1%) cases, tuberculous pleurisy – in 19 (23,2%) cases and other forms of TB (tuberculoma) – in 1 (1,2%) case. Association of 2 clinical forms met in 5 cases. Primary tuberculous complex and TB of intrathoracic lymph nodes were not diagnosed. Simultaneus extrarespiratory TB was diagnosed in 2 cases: 1 (1.2%) case with TB of mesenteric lymph nodes, 1 case (1.2%) with urogenital TB and TB of mesenteric lymph nodes.
Onset of illness with TB during pregnancy was acute in 31 (51.7%) pregnant women, subacute in 27 (45.0%) pregnant women and asymptomatic in 2 (3.3%) pregnant women. Bronchopulmonary complaints were seen in 60 (73.2%) pregnant women. In most of cases, the specific process has evolved under the mask of unspecific respiratory diseases such as pneumonia in 4 cases, bronchitis in 3 cases, acute viral infection in 2 cases. One case was disguised as early gestosis in the 1st semester of pregnancy.
Depending on localization, the TB process was spotted unilaterally in 60 (73.2%) cases and 22 (26.8%) cases bilaterally, and according to the expansion the TB process was limited to 1-2 segments in 47 (65.3%) cases and extended (≥3 segments) in 25 (34.7%) cases.
At the moment of delivery 60 (73.2%) pregnant women were BAAR-, 17 (20.7%) of pregnant women displayed BAAR+, 1 (1.2%) pregnant women – BAAR++ and 4 (4.9%) pregnant women – BAAR+++.
Assessment of extragenital pathology diagnosed in pregnant women under investigation, highlighted a high percentage of the excretory and urinary tract pathology in 15 – 18.3% of cases, in comparison to 7 (5.9%) cases of pregnant women from LM. Gastrointestinal diseases were displayed by 6 (7.3%) of pregnant women from LBA and 6 (5.0%) of pregnant women from LM. Diseases of the cardiovascular system were displayed statisticaly signifant more frequently by the pregnant women with sequelae of the tubercular process, in comparison to the pregnant women without tuberculosis – 7 (18.4%) and 5 (4,2%).
The analysis of pregnancy evolution established the high incidence of different complications in the group of pregnant women with active tuberculosis, in comparison to the group of the pregnant women without tuberculosis and group with post tuberculous sequelae (Table 1).
|
Table 1. Distribution of patients in study groups (%) according to the frequency of complications in the evolution of the present pregnancy. |
|||||
|
Complication of pregnancy |
Active TB group (n=82) |
TB sequelae group (n=38) |
No TB group (n=119) |
χ² |
p |
|
Imminence of early spontaneous abortion |
9 (11%) |
3 (8%) |
13 (11%) |
318 |
>0,05 |
|
Imminence of late spontaneous abortion |
15 (18%) |
5 (13%) |
4 (3%) |
12,467 |
<0,01 |
|
Imminence of premature birth |
23 (28%) |
9 (24%) |
8 (7%) |
17,409 |
<0,05 |
|
Pathology of fetus-placental system |
28 (34%) |
12 (32%) |
17 (14%) |
12,030 |
<0,01 |
|
Iron-deficiency anemia |
69 (84%) |
22 (58%) |
18 (15%) |
103,427 |
<0,001 |
|
Oedema in pregnancy |
3 (4%) |
4 (11%) |
4 (3%) |
3,621 |
>0,05 |
|
Early gestosis |
2 (2%) |
4 (11%) |
7 (6%) |
3,392 |
>0,05 |
|
Late gestosis |
4 (5%) |
2 (5%) |
6 (5%) |
1,875 |
>0,05 |
|
Total |
77 (94%) |
27 (71%) |
57 (48%) |
12,40 |
<0,001 |
|
Note: applied statistical test – χ². |
|||||
In pregnant women from LBA, a high frequency of iron deficiency anemia during gestation was found, in comparison to the pregnant women from LBS and LM (69 – 84.1%, 22 – 57.9% and 18 – 15.1%, respectively). This complication more frequently was developed in pregnant women in the second trimester of pregnancy from the LBA group (21 – 25,6%) and third (46 – 56,1%), in comparison to the pregnant women from the LBS group (0% and 5 – 13,2%) and pregnant women from LM (4 – 3,4% and 12 – 10,1%).
Following the study, the data acquired shows a high incidence of the feto-placental system pathology in pregnant women from LBA and in pregnant women from LBS, in comparison to the pregnant women from LM (28 – 34.1%, 12 – 31.6% and 17 – 14.3%, respectively) (Table 2).
|
Table 2. Distribution of women in study groups according to the complications of the fetus-placental system. |
|||||
|
Fetus-placental system complications |
Active TB group (n=82) |
TB sequelae group (n=38) |
No TB group (n=119) |
χ2 |
p |
|
Chronic FPI |
7 (9%) |
6 (16%) |
3 (3%) |
8,796 |
<0,05 |
|
Polyhydramnios |
3 (4%) |
2 (5%) |
1 (1%) |
2,974 |
>0,05 |
|
Olygamnios |
6 (7%) |
4 (11%) |
1 (1%) |
8,249 |
<0,001 |
|
IDDF |
21 (26%) |
6 (16%) |
14 (12%) |
12,812 |
<0,01 |
|
Chronic intrauterine hypoxia |
8 (10%) |
5 (13%) |
3 (3%) |
7,090 |
<0,05 |
|
Total |
28 (34%) |
12 (32%) |
17 (14%) |
11,489 |
<0,01 |
|
Notă: test statistic aplicat – χ². Note: applied statistical test – χ². |
|||||
In the structure of the feto-placental system pathology in pregnant women from LBA, it was recorded an increased incidence of the oligohydramnios, which is frequently associated with retarded foetus (6 – 7.3%) in comparison to LBS (4 – 10.5%) and LM (1 – 0.8%), RDIUF of hypotrophic type (18 – 22.0%); intrauterine chronic hypoxia (8 – 9.8%); chronic IFP (6 – 15.8%). Most of chronic IFP cases (5 – 50.0%) were diagnosed in the third trimester of pregnancy, being according to the clinical form and phase of active TB in the pregnant women from LBA.
For assessing the peculiarities of the delivery evolutions in women from the study groups, the following were studied: the term and way of finishing the pregnancy, duration of partuition per vias naturalis, incidence and structure of caesarean operations, labour complications.
The analysis did not find any statistically significant differences (p>0,05) in all study groups upon completion of pregnancy by delivery on term: 66 (80.5%) – in pregnant women from LBA, 33 (86.8%) – in pregnant women from LBS and 105 (88.2%) – in pregnant women from LM), though it was revealed a tendency of growth of this indicator in the in pregnant women without tuberculosis (Table 3).
|
Table 3. Distribution of patients in study groups (%) according to the term of birth. |
|||||
|
Term of birth |
Active TB group (n=82) |
TB sequelae group (n=38) |
No TB group (n=119) |
χ2 |
p |
|
Delivery at term |
66 (81%) |
33 (87%) |
105(88%) |
126,345 |
>0,05 |
|
Premature birth |
10 (12%) |
5 (13%) |
12(10%) |
6,803 |
>0,05 |
|
Post-term birth |
6 (7%) |
0 (0%) |
2(2%) |
1,131 |
>0,05 |
|
Note: applied statistical test – χ². |
|||||
In all the study groups prevailed the per vias naturalis conduct (78 – 95.1% in LBA, 97 – 81.5% in LM and 35 – 92.1% in LBS). Only 4 (4,9%) cases of LBA were finished with caesarean operation. The indications for caesarean operation were the following: apoplexia uteroplacentalis normally inserted, placenta praevia, breech position, fetal macrosomia with inssufciency of contraction forces, rebellious upon treatment.
In the group of patients with active tuberculosis prevailed the complicated delivery per vias naturalis, in comparison to the pregnant women without tuberculosis (56 – 71.8% and 51 – 52.6%), for this reason only approximately 1/3 of births were pshysiologic in the patients with active tuberculosis (22 – 28.2%).
Having analysed the clinical evolution of delivery in the studied groups, it was estimated an increased incidence of rapid and fulminant parturitions, insufficiency of primary and secondary contraction forces, RPPA, in patients from LBA. Based on the obtained data, was attested a high ratio of obstetrical trauma in pregnant women from LBA, in comparison to the pregnant women from LBS and LM (Table 4).
|
Table 4. Distribution of women in study groups according to the complications of labor and delivery period. |
|||||
|
Complication of labor |
Active TB group (n=82) |
TB sequelae group (n=38) |
No TB group (n=119) |
χ² |
p |
|
First period of labor |
|||||
|
RPPA |
27 (33%) |
10 (26%) |
32 (27%) |
1,005 |
>0,05 |
|
Primary insufficiency of the contraction forces |
8 (10%) |
0 (0%) |
0 (0%) |
15,848 |
>0,05 |
|
Secondary insufficiency of the contraction forces |
5 (6%) |
0 (0%) |
2 (2%) |
4,695 |
>0,05 |
|
Total of complications |
35 (43%) |
13 (34%) |
34 (29%) |
20,043 |
<0,05 |
|
Second period of labor |
|||||
|
Secondary insufficiency of the contraction forces |
2 (2%) |
0 (0%) |
0 (0%) |
3,862 |
>0,05 |
|
Rapid and fulminant delivery |
16 (20%) |
5 (13%) |
9 (8%) |
6,330 |
<0,05 |
|
Maternal obstetrical traumatism |
37 (45%) |
16 (42%) |
21 (18%) |
19,769 |
<0,001 |
|
Total of complications |
48 (59%) |
23 (61%) |
49 (41%) |
32,833 |
<0,05 |
|
Third period of labor |
|||||
|
Total of complications |
8 (10%) |
6 (16%) |
27 (23%) |
16,749 |
<0,001 |
|
Total of complications |
56 (72%) |
25 (71%) |
51 (53%) |
8,161 |
<0,01 |
|
Note: applied statistical test – χ². |
|||||
There were found no significant statistical differences (p>0.05) in the study groups regarding the total duration of delivery (527.3±24.3 minutes – in pregnant women with active tuberculosis of respiratory organs, 451.7±37.7 minutes – in pregnant women with sequelae of the tuberculous process and 556.9±18.6 minutes – in pregnant women without tuberculosis); duration of the second period of delivery (31.1±1.9 minutes – in pregnant women with active tuberculosis of respiratory organs, 31.7±3.7 minutes – in pregnant women with sequelae of the tuberculous process and 34.9±1.8 minutes – in pregnant women without tuberculosis). Approximately 1/3 of the patients from LBA the duration of delivery was up to 7 hours.
The average loss of blood in the natural delivery, was also similar in all study groups (284.2±12.6 ml – in pregnant women with active tuberculosis of respiratory organs, 267.1±19.1 ml – in pregnant women with sequelae of the tuberculous process and 289.8±15.3 ml – in pregnant women without tuberculosis), but it is worthy mentioning 2 cases of placenta adherens in LBA with a loss of blood of over 500 ml.
The assessment of postpartum period found complications (subfebrility, lochiometra, endometritis, mastitis, milk stasis, suture dehiscence) after parturition, statistically significant more frequent in the LBA group of pregnant women only, in comparison to the LM pregnant women (6 – 7.3% and 1 – 0.8%).
It has been considered that breastfeeding was allowed in 60 – 73,2% cases of pregnant women from LBA, in comparison to LBS and LM (36 – 94,8% and 119 – 100,0%, respectively). Breastfeeding was not allowed to mothers with HIV infection – 13.6% (3 cases), with MDR – 22.7% (5 cases), with BAAR+++ – 13.6% (3 cases), with BAAR+ with destruction and dissemination – 45.5% (11 cases).
Assessment of newborns characteristics, regarding the number of alive newborns, found no statistically significant differences in all study groups (81 – 98.8% in pregnant women with active tuberculosis of respiratory organs, 38 – 100.0% in pregnant women with sequelae of the tuberculous process and 119 – 100.0% in pregnant women with no tuberculosis), number of children born on time (72 – 87.8% in pregnant women with active tuberculosis of respiratory organs, 32 – 84.2% in pregnant women with sequelae of the tuberculous process and 105 – 88.2% in pregnant women without tuberculosis), number of children born prematurely (10 – 12.2% in pregnant women with active tuberculosis of respiratory organs, 6 – 15.8% in pregnant women with sequelae of the tuberculous process and 12 – 10.1% in pregnant women without tuberculosis).
In Table 5 is displayed the analysis of children prematurely born according to the term of gestation.
|
Table 5. Distribution of the premature new borns in the patients of the study group (%) according to the gestation period. |
|||||
|
Gestation term |
Active TB group (n=82) |
TB sequelae group (n=38) |
No TB group (n=119) |
χ² |
p |
|
26-28 weeks |
1 (10%) |
2 (40%) |
1 (8%) |
1,328 |
<0,05 |
|
29-30 weeks |
0 (0%) |
0 (0%) |
1 (8%) |
0,191 |
<0,05 |
|
31-33 weeks |
3 (30%) |
1 (20%) |
5 (42%) |
1,693 |
>0,05 |
|
34-36 weeks |
6 (60%) |
2 (40%) |
5 (42%) |
1,327 |
>0,05 |
|
Total of premature births |
10 (12%) |
5 (13%) |
12 (10%) |
4,903 |
>0,05 |
|
Note: applied statistical test – χ². |
|||||
Assessment of the newborns’ condition upon birth was made under Apgar score. Based on the obtained data, in most of the cases, the general condition of the children included in the study was satisfying. Great parts of them were given 7-8 points under Apgar score (Table 4). In one case in the study group, was ascertained the intranatal death of the premature fetus with the weight of 1248 g.
A special moment that has a direct influence on the perinatal indicies belongs to the body weight of the new borns upon birth. Following the study it was found, that most of the children born in all the study groups had a bodily weight of over 3000 g. At the same time, in LBA, every 7th child was born with the weight of <2500 g, 5 – 6,1% children with the weight under 2000 g and 6 – 7,3% children with the weight within the limits 2000-2499 g. Additionaly, during the research, it has been outlined that the small weight of the newborns (<2500 g) decreases proportionally according to the clinical form and phase of the TB process, as well as duration of the treatment: the more active the specific process was and the treatment prescribed was not observed, the more frequent was the incidence of births with small foetuses, less than 2500 g, fetal suffering was more pronounced and the risk of developing RDIUF was higher.
|
Table 6. Distribution of the premature new borns in study groups according to the Apgar score in the first minute of life. |
|||||
|
Apgar score in the first minute of life |
Active TB group (n=82) |
TB sequelae group (n=38) |
No TB group (n=119) |
χ² |
p |
|
8-10 points |
50 (62%) |
23 (61%) |
55 (46%) |
11,653 |
>0,05 |
|
6-7 points |
28 (35%) |
12 (32%) |
59 (50%) |
6,029 |
>0,05 |
|
1-5 points |
3 (4%) |
3 (8%) |
5 (4%) |
1,128 |
>0,05 |
|
Note: applied statistical test – χ². |
|||||
The vaccination rate with BCG on the 2nd day of life, was statistically significantly lower in the group of pregnant women with active tuberculosis of respiratory organs, in comparison to the pregnant women without tuberculosis (69 – 85.2% și 116 – 97.5%); in the group of pregnant women with sequelae of the turberculous process, in comparison to the pregnant women without tuberculosis, (31 – 81.6% și 116 – 97.5%). Vaccination has not been carried out to 12 – 14.8% children in LB, as contraindications there were intrauterine infectious pneumonia, intrauterine infection, severe neonatal jaundice. It is important to mention that upon vaccination with BCG of children born from mothers with active TB, the bacillary status of the mother has not been taken into account, as the data of the specialized literature and international protocols reported.
Analysis of early postnatal losses in weight in newborns ascertained that approximately 1/3 of children born from LB displayed pathologic postnatal weight losses, in comparison to the pregnant women with sequelae of the tuberculous process (25 – 30.9% and 4 – 10.5%), and pregnant women without tuberculosis (25 – 30.9% and 6 – 5.0%, respectively).
TB has a negative impact on the condition of the new born, which was characterized by increased incidence of perinatal morbidity (Table 7).
|
Table 7. Structure of the neonatal pathology in newborns from the study group. |
|||||
|
Complication of the fetus-placental system |
Active TB group (n=82) |
TB sequelae group (n=38) |
No TB group (n=119) |
χ² |
p |
|
Intrauterine infection |
9 (11%) |
5 (13%) |
0 (0%) |
15,071 |
<0,01 |
|
Aspiration syndrome |
5 (6%) |
0 (0%) |
0 (0%) |
9,899 |
<0,01 |
|
Congenital developing anomalies |
4 (5%) |
2 (5%) |
0 (0%) |
6,166 |
<0,05 |
|
Birth traumatism |
2 (3%) |
0 (0%) |
0 (0%) |
3,909 |
>0,05 |
|
Cefalohematoma |
2 (3%) |
0 (0%) |
3 (3%) |
0,971 |
>0,05 |
|
Post-hemorrhagic anemia |
1 (1%) |
0 (0%) |
0 (0%) |
1,946 |
>0,05 |
|
Aspiration pneumonia |
8 (10%) |
3 (8%) |
0 (0%) |
11,763 |
<0,01 |
|
RDIUF |
20 (25%) |
6 (16%) |
15 (13%) |
5,003 |
<0,01 |
|
Hemorrhage / peripheral ischaemia |
20 (25%) |
7 (18%) |
14 (12%) |
5,693 |
<0,01 |
|
Cardiac pathology |
1 (1%) |
0 (0%) |
0 (0%) |
1,946 |
>0,05 |
|
Total |
40 (50%) |
16 (42%) |
27 (23%) |
16,161 |
<0,001 |
|
Note: applied statistical test – χ². |
|||||
Congenital abnormalities of development were found statistically significantly more frequent in the group of pregnant women with active tuberculosis of the respiratory organs, in comparison to the pregnant women without tuberculosis (4 – 4.9% and 0 – 0%). Of all congenital abnormality cases found, in only one case the specific tuberculous treatment with drug preparations of the first line was administered in the first trimester of pregnancy, developing medication fetopathy with heart malformation in the newborn. In the other cases the the specific treatment was administered starting with the third trimester of pregnancy, when the possible embrio- or foetotoxic impact of antituberculous drugs has already passed.
Discussion
The obtained data are concorded with the data of the foreign scientists (Mnyani C., McIntyre J., 2011) which underlines the increased incidence of the pregnancy and delivery complications in women with active tuberculosis of the respiratory organs [2]. According to the bibliographic sources (McCarthy F. et al., 2006) the complicated evolution of pregnancy and delivery of this contingent of women is found in 40,0-43,1% cases, and according to the data obtained – up to 70% cases [12].
The frequency of iron deficiency anemia among pregnant women with active tuberculosis of respiratory organs (according to the data obtained approximately 80%) is much more increased than the average in population (15-20% according to the Loto O., Awowole I., 2012). The tuberculous intoxication of the woman’s body and consumption of iron necessary for the development of the fetus have determined this [10].
Due to insufficient saturation of blood with oxygen and tissue hypoxia in pregnant women with active tuberculous process appears the cardiopulmonary insufficiency, which determines the development of feto-placental insufficiency and increase of the incidence of intrauterine growth retardation of the fetus [13, 14].
According to Ghosh K. et al. (2011), one of the most frequent complications of the labour in the studied contingent of patients is the premature rupture of the amniotic sac, caused by the infection of the amniotic membranes and decrease of their resistance [6]. The results of our research confirmed this data and acquired an incidence of 32.9%.
Pillay T. et al. (2004), same as the results of herein research, suggest the decrease of total delivery duration and increase of the number of rapid and precipitated deliveries, accompanied by the increased incidence of the fetal and maternal postpartum trauma [15].
According to the data of Ghosh K. et al. (2011), as well as those acquired by us, the tuberculous process is found more frequently among multipara and more rarely among primiparae [6].
The analysis of the extragenital anamnestic peculiarities has significantly found more frequently diseases of the respiratory system, cardiovascular system, excretory and urinary system, chronic diseases of the liver and tobacco smoking in pregnant women with active tuberculosis of the respiratory organs in comparison to the pregnant women without tuberculosis. Has been gound a direct correlation between the clinical form and active tuberculosis phase and degree of iron deficiency anemia during gestation.
Analysis of present pregnancy evolution found complications (feriprive anemia, imminence of spontaneous abortion, and imminence of preterm parturition) more frequently in pregnant women with active tuberculosis of respiratory organs and pregnant women with sequelae of the tuberculous process, in comparison to the pregnant women without tuberculosis.
The evaluation of neonates has diagnosed neonatal pathologies, such as intrauterine infection, aspiration syndrome, congenital anomalies of aspiration pneumopathy development, haemorrhage / peripheral ischaemia, ischaemic hypoxic encephalopathy and RDIUF more frequently in the group of pregnant women with active tuberculosis of respiratory organs, in comparison to the pregnant women without tuberculosis.
The research highlits new pregnancy evolutive peculiarities with TB background of respiratory organs, fact which facilitates the understanding of physiological mechanisms as well as of the pathological ones that happen in the pregnant woman’s body with or without TB, a moment of great importance in a correct approach of the conduct tactics of pregnant women and neonates with active TB. The obtained data, during the research shall complete the knowledge of the obstetrician-gynecologist doctors on the conduct algorithm in preganant women with TB, both in the practical sector and in the medical institutions of the second and third levels of perinatal medical assistance.
In comparison to the researches quoted in the paper, our study was a retrospective one. Extracting data from the medical documentation, which was filled up by different medical staff, could be considered also, a bias factor.
Conclusions
When studying pregnancy evolutive peculiarities it was found that the ratio of pregnancy complications in pregnant women with active tuberculosis is a superior index, in comparison to that from the witness group. In patients with active tuberculosis twice more frequently complications were recorded (feriprive anemia, imminience of late spontaneous abortion, imminence of preterm parturition) and 2.4 times more frequent diseases of the foeto-placental system (oligoamnios, RDIUF of hypotrophic type, intrauterine chronic fetal hypoxy). This fact confirms the pathogenetic relationship of complications in pregnancy with tuberculous intoxication.
The research carried out provides data about the repercurssions of active TB on delivery and labour. The pregnant women with active TB displayed a more complicated evolution of delivery: RPPA – 4 times more frequently, rapid and fulminant delivery – 2.6 times more frequently, maternal obstetrical trauma – 2.6 times more frequent, insufficiency of contraction forces – 9 times more frequent. Thus, only approximately 1/3 of deliveries were physiological in patients with active TB.
The realised study demonstrated that the maternal active tuberculosis has a negative impact on neonates, characterized by the increased incidence of RDIUF, aspiration syndrome, aspiration pneumopathy and intrauterine infection.
Declaration of conflicting interests
Nothing to declare.
Authors' contribution
Both authors contributed equally to the research, data analysis, writing and reviewing of the manuscript. Both authors read and approved the final version of the article.
REFERENCES
- Jana N., Barik S., Arora N. Tuberculosis in pregnancy – a major maternal and perinatal challenge. BJOG, 2011; 118 (9): 1145-1146.
- Mnyani C., McIntyre J. Tuberculosis in pregnancy. BJOG, 2011; 118 (2): 226-231.
- Lin H., Lin H., Chen S. Increased risk of low birthweight and small for gestational age infants among women with tuberculosis. BJOG, 2010; 117 (5): 585-590.
- Moga M., Bâgiu N., Pascu A. et al. Postponement of pregnancies in women with tuberculosis. Bulletin of the Transilvania University of Braşov. Series VI: Medical Sciences, 2013; 6 (1): 49-58.
- Bekker A., Schaaf H., Draper H. et al. Tuberculosis disease during pregnancy and treatment outcomes in HIV-infected and uninfected women at a referral hospital in Cape Town. PLoS One, 2016; 11 (11): e0164249.
- Ghosh K., Ghosh K., Chowdhury J. Tuberculosis and female reproductive health. J. Postgrad. Med., 2011; 57 (4): 307-313.
- Ngwenya S. Tuberculosis in pregnancy: delayed diagnosis, lost lives. Pulm. Res. Respir. Med. Open. J., 2016; 3 (3): 37-40.
- Ali A., Abdallah T., Rayis D. et al. Maternal and perinatal outcomes of pregnancies associated with tuberculosis in eastern Sudan. Int. J. Gynaecol. Obstet., 2011; 114 (3): 286-287.
- Mayer K., Mathad J., Gupta A. Tuberculosis in pregnant and postpartum women: epidemiology, management, and research gaps. Clin. Infect. Dis., 2012; 55 (11): 1532-1549.
- Loto O., Awowole I. Tuberculosis in pregnancy: a review. J. Pregnancy, 2012; article 379271.
- Keskin N., Yilmaz S. Pregnancy and tuberculosis: to assess tuberculosis cases in pregnancy in a developing region retrospectively and two case reports. Arch. Gynecol. Obstet., 2008; 278 (5): 451-455.
- McCarthy F., Rowlands S., Giles M. Tuberculosis in pregnancy – case studies and a review of Australia's screening process. Aust. N. Z. J. Obstet. Gynaecol., 2006; 46 (5): 451-455.
- Clinical Practice Guideline on the Diagnosis, Treatment, and Prevention of Tuberculosis. Ministry of Science and Innovation, Spain, 2010. 222 p.
- Whittaker E., Kampmann B. Perinatal tuberculosis: new challenges in the diagnosis and treatment of tuberculosis in infants and the newborn. Early. Hum. Dev., 2008, 84 (12): 795-799.
- Pillay T., Khan M., Moodley J. et al. Perinatal tuberculosis and HIV-1: considerations for resource-limited settings. Lancet Infect. Dis., 2004; 4 (3): 155-165.
